San Francisco Chronicle Magazine
UCSF is at the forefront of studying frontotemporal dementia, a wasting disease similar to Alzheimer’s that strikes patients at their peak.
Dawn spoke with impeccable grammar until she reached her late 40s, when she began struggling to assemble a sentence. Her 8-year-old daughter would ask for a hug, but the once-doting mother pushed her away. A former vice president at a local bank, Dawn became unable to manage her own finances. Her spending became so irrepressible that her family had to seek court orders to prevent her from losing everything she had saved. Before she was diagnosed with frontotemporal dementia (FTD) at the University of California at San Francisco in 2002, Dawn divorced her husband. She was 52 years old. And the relentless decline continued.
“I do a lot of crying,” says Dawn’s mother, Emmogene, who lives in Antioch, cares for a husband with early Alzheimer’s disease and regularly attends UCSF’s FTD caregiver support group meetings. “It’s been really hard because you think you’re going to die before your children. You just have to go through it a day at a time, thinking about how they were and how they are now, and feeling so helpless.”
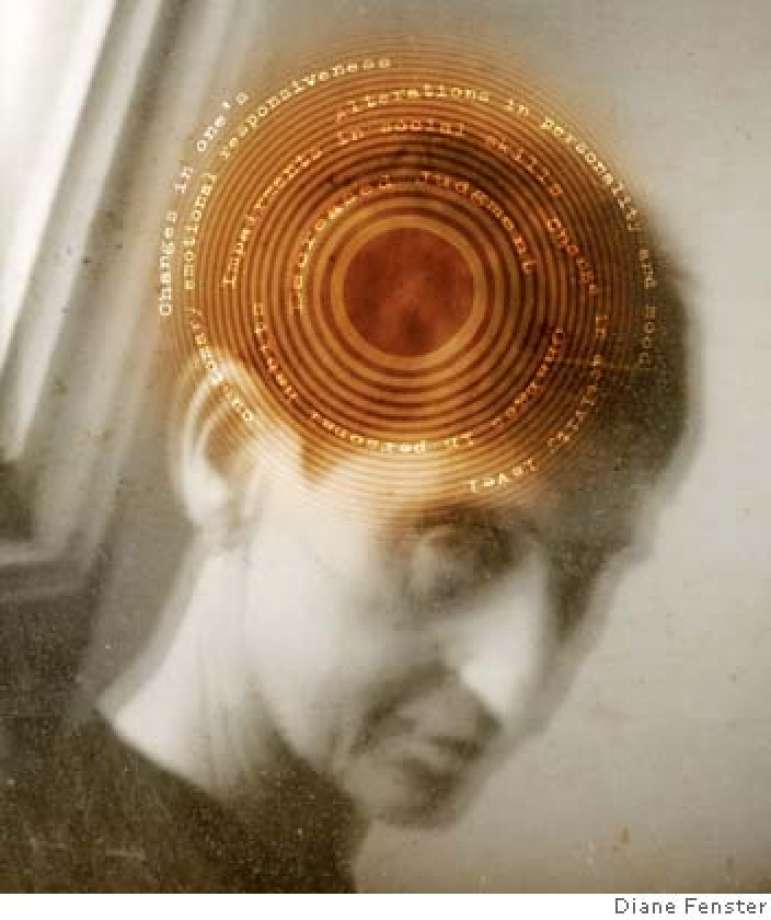
Financial mismanagement and loss of judgment and empathy are typical symptoms of frontotemporal dementia, a degenerative brain disease that attacks slowly and yields devastating results, often stripping patients of language skills and inciting behavior so bizarre, damaging and unpredictable that approximately 60 percent of cases are misdiagnosed as psychiatric disorders. Perhaps even more catastrophic is the loss of personality — the relentless destruction of everything that made someone who he or she once was — which often obliterates relationships and careers before anyone even determines there is an illness.
“I think this disease is so much harder on the family than on the patient,” says Jennifer Merrilees, a nurse who led UCSF’s FTD caregiver support group and is now earning her doctoratein nursing and geriatrics. “The family deals with so much heartache, and so much of the unknown. It’s a maze.”
Frontotemporal dementia, also known as frontotemporal lobar degeneration (FTLD), has not become everyday terminology — yet. But it’s on the brink of public awareness in the same way Alzheimer’s disease was 20 years ago. The scientists and physicians at UCSF are on the forefront of exploring an illness they believe to be more common than anyone has realized.
Experts regard FTD as the second most prevalent cause of dementia behind Alzheimer’s, which ails an estimated 4.5 million people in the United States. But FTD’s economic and emotional consequences are more detrimental, because it strikes otherwise healthy individuals in their 40s, 50s and early 60s, who are often at the peak of their careers and parenting responsibilities. There is no known cause, no treatment and no cure. Genetics may be responsible for 40 percent to 50 percent of cases. The rest appear to be random.
One barrier to public knowledge about FTD is that it can’t be reduced to “10 early-warning signs.” Though many similarities with Alzheimer’s disease exist, the key difference is that FTD patients display only limited memory loss. Results of intelligence tests can remain normal, and individuals with unimpaired motor control can stay athletic for a long time, conveying the illusion of good health.
Even in the Bay Area in an era of AIDS and Alzheimer’s, the social stigma associated with a little- understood dementia makes coping even more challenging for families.
This is something those participating in UCSF’s monthly FTD caregiver support group meeting understand intimately. At a recent gathering in a small hospital conference room, the family of a newly diagnosed FTD patient intends, for the first time, to seek answers from people who have been dealing with the illness for as long as 10 years.
Frustration, tears, resignation and a remarkable desire to offer helpful advice fuel the unsteady emotional energy in the room, where 15 people crowd around a long table.
“I lost my husband, but I’ve been given another person I don’t like,” one woman says. Everyone nods in agreement.
Another adds, “You have a big baby who can’t learn anything.”
Phrases such as “the decision-making powers have gone to hell in a handbag,” “no impulse control,” “I don’t know who this person is,” “whatever seems like the hugest problem now won’t be in a few months,” “perpetual state of grieving” and “it’s very, very hard to watch,” are just some of the statements uttered.
The new family members explain their struggle with the patient’s actual competence level and his perceived abilities. Driving, working and interpersonal relationships have become battlegrounds. “We’re still trying to reason with him,” says one, before adding softly, “but there’s no reasoning with him.”
In a sympathetic tone, the entire group confirms, “No.” The patient’s wife, attending the support group meeting without his knowledge, quietly intercepts her tears before they fall.
From the other end of the table, a word of encouragement emerges: Ask for help, because “it’s amazing the kind of support you’re going to get from the least likely places.”
But asking for help is not easy when a definitive diagnosis remains elusive. In fact, the only way to know for sure if a patient has FTD is by examining his brain after he’s died. This is not the case with Alzheimer’s, which clinicians can pinpoint with more confidence.
“The whole idea of the first symptom is a moving target,” says Merrilees. It’s almost always something that’s understood long after it occurs — even years later — when spouses begin to comprehend the disease and re-examine strange behaviors they once tried to ignore or attribute to stress.
Consequently, detecting FTD remains more of an art than science. Magnetic resonance imaging and CT scans can help rule out a brain tumor and reveal cerebral atrophy, but these and PET scans “are not a means for making a diagnosis,” says Tiffany Chow, a neuroscientist at the University of Toronto and a speaker at UCSF’s FTD conference in September. Neuropsychological tests can help, but Chow says that nothing is more effective than a complete examination and history of speech impairments and/or behavioral changes.
Information from patients is notoriously unreliable. They may admit to minor limitations, but as the disease progresses, a lack of insight prohibits them from recognizing, or caring about, their deficiencies.
Compounding the problem is the fact that primary-care physicians and neurologists in private practice may have limited knowledge of the disease and difficulty obtaining information. The patient may block communication between the physician and other family members. Or families might be reluctant to tell the truth, out of embarrassment or fear of repercussions from a now-volatile loved one.
“I can’t tell you how many times before someone ever visits us, things are ruined,” says Dr. Bruce Miller, director of UCSF’s Memory and Aging Center. “Patients may be able to say the difference between right and wrong, but they don’t know the difference between right and wrong.”
Unmonitored patients often get arrested for erratic driving or theft, or wreak havoc in the home and workplace with inappropriate behavior, sexual or physical aggression, or gross financial mismanagement. Others may just sit home and play solitaire all day, a type of apathy that can be “extremely stressful for families,” according to Merrilees. No matter what the circumstances, “there’s a relentlessness to what (the caregiver) is going through, and that’s really hard to shoulder.”
Jan, who lives in Berkeley with her husband, an FTD patient, puts it more bluntly. “You don’t get any affection,” she says. “You lose your sense of touch. They’re not really there. It’s like there’s been a terrible automobile accident, and suddenly I have to take care of a very bizarre child with brain damage.”
Like others interviewed for this story, Jan asked that only her first name be used. Some feared angering or embarrassing their loved ones; others expressed concern that people might try to take advantage of the gullible FTD patient.
Which parts of the brain make us ourselves? “Those are the parts even the most skilled neurologists still don’t understand very well,” says Howie Rosen, a neurologist at UCSF.
Consequently, knowledge about the cause of the illness is limited and constantly evolving. Essentially, misfolding proteins aggregate and become like sludge or tangled train tracks that cause horrific wrecks in the brain.
Abnormal deposits of the tau protein (also present in Alzheimer’s and Parkinson’s diseases) can be one source. Another cause is a deficit of the progranulin protein — essential for neuron survival. This leads to pathological deposits of ubiquitin, a protein recently identified as TDP-43, which is also present in ALS, or Lou Gehrig’s disease.
New discoveries prove that this illness is not as isolated as scientists once thought it was. “If you look at a tiny piece of it, like the tail of an elephant, you see a rare disease,” says Miller. “But if you combine all the diseases together as they’re linked, you really get an elephant — a disease that’s very common.”
Though some literature indicates an equal number of men and women have FTD, the ratio of male to female FTD patients at UCSF is two to one. Initial symptoms may include language difficulties, behavioral anomalies or both. Typically, clinicians try to control behavior — often with antipsychotic medication that works sporadically. Patients die from complications of the illness within three to 15 years.
Caregivers often express frustration that doctors can’t visit their homes for extended periods to see what happens behind closed doors.
“I wish these people had more time to observe,” says Don (his name has been changed for privacy reasons), who brought his 49-year-old wife in for evaluation at UCSF. “I’m not really sure they’re getting a full picture.”
Miller says they will make house calls to noncompliant patients. But too few experts and a constant scramble for resources make this kind of care impossible for everyone.
UCSF’S Memory and Aging Center is located on the Parnassus campus, with views of Golden Gate Park. Its $8 million annual operating budget comes from grants, including two from the National Institutes of Health. Local philanthropy — such as the Hillblom, McBean and Koret foundations — provides one-fourth of that. Miller would like to see those numbers rise.
“Private funding comes with fewer strings attached, and it allows us to do really creative things,” he says.
UCSF is also working on a promising video about FTD that the school hopes to air on PBS in the next two years. But its completion awaits donations.
When Miller became the leader of UCSF’s Memory and Aging Center in 1998, there were three employees. Now, 70 people share space meant for half as many. When someone enters the lobby area, those waiting in chairs must turn their legs to the side to let the person pass.
What makes Miller adept at managing an illness with so few boundaries is his ability to veer from conventional wisdom. “I have my own way of thinking about things,” he says. “I’m eager to improve what we do every week, and I’m comfortable with people — and unconventional. I don’t necessarily follow the well-beaten path. Because if you think that by doing routine tests you’re going to understand this disease, you’re wrong. You have to explore somebody’s life and think about what’s unusual about it, even if it’s exemplary.”
A leader who educates physicians and scientists around the world, Miller evaluates 75 patients a year, up from 15 or 20 when he first began studying FTD in 1984.
On a typical day, he gathers a few members of his team in his cramped office, decorated with family photos and a plastic model of the brain, to discuss a patient named Olivia (not her real name). Dressed in a pinstriped suit, the 57-year-old physician-scientist invites input from clinical nurse Robin Ketelle; physician Huidy Shu, Katie Carey, a neuropsychology fellow; and Lovingly Quitania, a graduate student in neuropsychology.
FTD is commonly misdiagnosed as Alzheimer’s, bipolar disorder or schizophrenia, and this patient is no different. Though MRIs can often appear normal, Miller examines images of her brain on his computer. He comments on the atrophy in the frontal lobe, and explains how he will superimpose the new image over a year-old picture and statistically calculate any change.
Before this meeting, Olivia’s husband, Don, explains privately that she had been a “superwoman” who managed her work and motherhood responsibilities with ease. “She was really at the top of her game,” he recalls wistfully.
But when she was 44, her behavior began to change. She exhibited unusual fits of anger and agitation, which sent the couple to a marriage counselor. “What I didn’t realize at the time was that she was also having anger management issues at work,” he says. “But it was easy to attribute that to stress.”
Things got worse. She obsessed about certain topics, and conversations became laborious as she repeated herself incessantly. She drove the wrong way down a one-way street. Multitasking became impossible. Affection for everyone in the family diminished. A trip to the store yielded 24 cans of shaving cream and towels the family didn’t need. Unable to monitor her eating, her weight fluctuated dramatically.
The marriage counselor thought she was depressed, and “the psychiatrist was a disaster,” says Don. He was never sure if her peculiar behavior — like weeding the garden at 3 a.m., naked — was due to the illness or the medications prescribed for her. Two years before her diagnosis, she was fired from her job for poor performance, though she denied any wrongdoing. She found another job, and promptly was terminated from that as well. Reports indicated that she didn’t understand instructions, or couldn’t execute them. In 2005, the couple finally got some answers at UCSF.
“The hardest part is losing my wife a little bit at a time,” Don says. “It makes me live in a perpetual state of unresolved grief.” Despite the support from his community and church, “it still hurts, and it’s still a struggle to go through. I feel like she’s mostly gone. Her personality is completely different. There are times when I catch myself sort of acting like she’s still the same person, and that usually gets me knocked down really hard. It doesn’t work. But when there’s this glimmer of a response that reminds of the way she used to be, I’ll try to respond to that, and it meets a brick wall.”
Following the one-hour summary of Don’s observations, the team walks from Miller’s office to the hospital, where Olivia and Don are waiting.
In front of his wife, however, Don is guarded. He knows that saying anything she doesn’t like will result in a disturbing encounter later on, sans witnesses.
With an audience of six, Miller shifts between neurological exams and light conversation with Olivia in an unassuming, accessible, respectful manner that seems to put her at ease. Because many of his patients have trouble talking, Miller has perfected the art of multifaceted communication.
“I feel I’m in the presence of a master when he is working with patients,” notes Ketelle. “He listens and responds on a nonverbal level that I find unorthodox and very effective.”
Clinically, Miller is analytical in an intuitive way that comes from 23 years of studying an illness most doctors do not yet understand.
With arms crossed, Olivia admits that her personality might have changed “a little bit.” She knows she repeats herself, and that she’s not “wonder woman anymore.” But that’s all she seems to grasp. Miller adjusts easily to the irregular terrain.
FTD patients lack judgment in a way that makes them unable to recognize their own deficiencies or appreciate threats to their safety — or the safety of others. Their ability to appear lucid and competent much of the time makes them a challenge to manage.
“With FTD, we see families in major crisis,” says Geri Hall, a featured speaker at UCSF’s International FTD Conference in September, and an advance-practice nurse in Iowa who has seen the damage after working with hundreds of FTD patients. “The problem is that the patient has not been determined to be incompetent, and nobody wants to take away the autonomy of someone who is not impaired. So the caregiver is constantly being barraged by negative restrictive feedback that he is trying to limit this competent person. It’s like swimming in one of those endless pools.”
Miller and his team are trying to change that by focusing on collaborative work that advances everyone’s understanding of the disease — and by treating real people on a daily basis. He also devotes much of his 100-hour weeks to fostering the next generation of clinical researchers.
His much-publicized exploration of the artistic talents elicited in many FTD patients is a testament to his ability “to recognize something beautiful that has come out of something horrible,” says clinical behavioral neurology fellow Brandy Matthews. “It’s just a different way of thinking about a disease process that’s very unique to him. It takes some asking to figure out what (patients) still do well, and he always focuses on that.”
While Miller and his team hunt for treatment and a cure, family members struggle with overwhelming barriers and limited options. Nursing homes become problematic when young and physically able patients are too strong for staff members prepared only for the frail elderly.
Jan recalls her efforts to find day care for her 6-foot-4-inch husband while she went to work in the city. When she finally placed him, he demanded to go home on the first day. The staff politely and quickly escorted him to the door.
When she isn’t busy explaining FTD to her therapist, she’s working to make ends meet. Of the $5,000 a month Jan brings home, $4,500 now goes to caregivers, whom she pretends are artists looking for space, or people who want help running errands so he will allow them to stay. But she believes it’s essential to give her the respite she needs to survive.
“We rent videos because we can’t afford to go to the movies,” she says. “Plus, I have to do hours of work just to come into the office. But having a human being who does not have dementia to talk to is really important.” The most difficult part is dealing with the “ocean waves of emotional grief. For years, I’ve had a bad cry every week — sometimes more. It’s like you’re slogging through mud, the mud being all the emotions that drag you down. You gradually shut down and become not really alive.”
Emmogene, who talks about her daughter, Dawn, in UCSF’s caregiver support group meetings, understands this anguish.
These days, Dawn does not speak at all. She’s incontinent, but fights every attempt to clean and bathe her. Her once-energetic walk has become a shuffle, but she paces constantly, and when she tries to sit down, she sometimes falls and hurts herself. Even with constant monitoring from family and a professional caregiver, she’s managed to shoplift a few items, which her family must return with a written note from doctors, along with profuse apologies. Antidepressants and antipsychotic drugs that seemed to help temporarily have fallen by the wayside as the benefits became undetectable, and side effects, like diarrhea, became impossible to manage. Emmogene pays lawyers and accountants tens of thousands of dollars to maintain control over Dawn’s finances.
Echoing the sentiments of every loved one and physician dealing with FTD, Emmogene’s voice breaks as she whispers, “I just wish I could do something for her.”
Help for caregivers
Frontotemporal dementia (also called frontotemporal lobar degeneration) is an umbrella term that covers several disease subtypes. They are named according to the way the disease began. Doctors agree that, as each one progresses, the severity of symptoms may vary, but they all begin to resemble one another.
Primary progressive aphasia or progressive non-fluent aphasia: Begins with language disorder and may remain isolated there for up to two years. All patients suffer behavioral symptoms and cognitive decline as the disease spreads.
Semantic dementia: Language problems initially, primarily with comprehension.
Pick’s disease: Immortalized in a tragic plot turn in Sue Monk Kidd’s “The Mermaid’s Chair” and first described by Arnold Pick in 1892. Behavioral symptoms exhibited first.
Corticobasal degeneration: Begins with motor control and coordination problems.
Progressive supranuclear palsy: A related disorder that begins with problems with gait and balance.
On the Web
University of California San Francisco Memory and Aging Center:www.memory.ucsf.edu(includes information about support group meetings)
Association for Frontotemporal Dementias: www.ftd-picks.org; (866) 507-7222.
In print
“What If It’s Not Alzheimer’s: A Guide to Dementia,” by Lisa Radin
Support Group
Available monthly, second Thursdays, 1:30-3 p.m., call Robin Ketelle, RN, MS; (415) 502-1053, rketelle@memory.ucsf.edu; UCSF Ambulatory Care Clinic (ACC) Building, 400 Parnassus, 8th Floor, Neurology Conference Room.