Dementia
Understanding Dementia
As a writer and journalist who has lost loved ones to dementia, my primary objectives in sharing personal accounts — mine, with my husband and father, and those of others — are to help strengthen awareness and sensitivity for people living with and around dementia, reduce stigma and isolation, and change the way we understand and manage dementia in both daily life and the practice of medicine.
The World Health Organization declared dementia a public health priority — in 2012. And it’s only becoming more acute. Neurological illnesses know no geographic, racial, or socio-economic barriers. Nor are they limited to genetic predisposition. Not one of us is immune.
In my ongoing efforts to illuminate the hidden ways that dementia-related illnesses impact lives, I’m writing a narrative nonfiction book, which expands on articles I’ve researched and written for New York Magazine / The Cut, New York Times Magazine, San Francisco Chronicle Magazine, Canadian Journal of Neurological Sciences, and other publications.

Alzheimer’s disease is the leading cause of dementia, so it’s a vital part of the discussion. Comparatively, much less has been written about non-Alzheimer’s dementias — some of which strike people when they’re younger, at the peak of their careers. Wider recognition is essential for many reasons, especially because it can decrease the shame that also prevents people from finding help. I hope this book clarifies non-Alzheimer’s dementias for those less familiar, while also elucidating possible ramifications that some experts might not have considered.
Another purpose is to inspire conversations with family and friends about what we want in life and death, and everything in between — should we ever lose the capacity to make those decisions for ourselves. As noted above, there are no guarantees for any of us. So we would do well to share our truth, lose the shame, articulate what we want for our own lives long before we think we should, advocate for each other, and become better listeners. Because these experiences are not as unique as we’d like to think, and nobody should have to go through them alone.

Brief Overview of Dementia
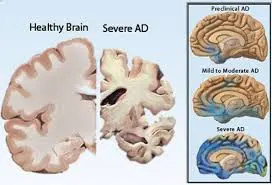
Dementia is defined as a constellation of symptoms that degenerates over time. Different causes affect various parts of the brain, which result in some notable distinctions.
Illnesses that may cause dementia include Alzheimer’s disease, Lewy body dementia, frontotemporal dementia, vascular dementia, progressive supranuclear palsy, and corticobasal degeneration, among others.
What are the sources these diseases? A combination of genetic, environmental, and lifestyle (diet, exercise, stress) factors, along with each person’s unique predisposition for a particular illness. We know a lot about what we can do to improve our chances of staying healthy, but much remains a mystery about why one family member develops a disease and another, who lives a similar lifestyle, may not.
Here’s an overview of the most common illnesses that cause the cognitive decline of dementia:
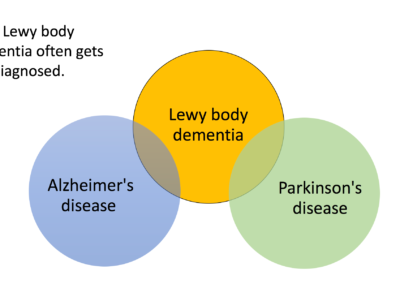
Lewy body dementia (LBD) or Dementia with Lewy bodies (DLB)
Personal observations: When my father first began showing signs of dementia, nobody could pinpoint the source of the problems. Issues with attention and memory resembled Alzheimer’s disease. Vivid recollections from his football days in high school and college were readily available, yet he couldn’t remember new material for volunteer work. Yet the forgetfulness was inconsistent. As a collegiate (and lifelong) athlete and former Navy SEAL, Dad’s trouble with balance, coordination, and handwriting raised suspicions of Parkinson’s disease. But there was no obvious tremor. Besides, that explanation seemed incomplete. He struggled to sleep, so a neurologist prescribed a C-PAP machine. Conversations shifted to sleep apnea, Post-Traumatic Stress Disorder (he fought in the Vietnam war), and mild cognitive impairment, which also seemed inadequate, given the disturbing hallucinations that upset him (and everyone else) more frequently.
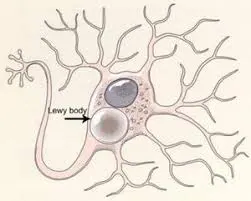
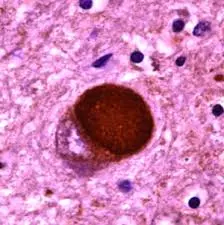
I started calling the primary care physician to make sure he had all the information about what had been happening. But he didn’t, because reports to him had been incomplete or well-burnished. We suspected Lewy body dementia. Pink blobs deposited in the brain are the Lewy bodies that give the disease its name. These are different from the tumbleweeds that are the abnormal amyloid of Alzheimer’s disease.
We finally confirmed the illness — in the autopsy after he died.
From the textbooks: Lewy body dementia (LBD) is a disease associated with abnormal deposits in the brain of a protein called alpha-synuclein. These deposits, also called Lewy bodies, affect chemicals whose changes, in turn, can lead to problems with thinking, movement, behavior, and mood. This is one of the reasons why it can be misdiagnosed for a psychiatric illness such as schizophrenia. LBD is one of the most common causes of dementia, after Alzheimer’s disease and vascular disease.
(Source: National Institute on Aging at the National Institutes of Health)
In our video, behavioral neurologist Tiffany Chow, M.D. calls LBD (or DLB – don’t let the acronyms get you down) a terrible mash-up of Alzheimer’s and Parkinson’s’ diseases.
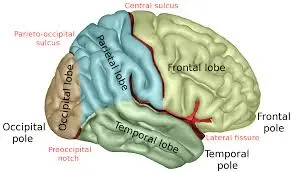
Key parts of the brain involved:
- Cerebral cortex (information processing, perception, thought, language)
- Limbic cortex (emotions and behavior)
- Hippocampus (forming new memories)
- Mid-brain and basal ganglia (movement)
- Brain stem (regulating sleep and alertness)
(Source: National Institute on Aging, National Institutes of Health)
More information and help:
Th Lewy Body Dementia Association website contains videos of lectures and webinars with experts. Because LBD differs from other forms of dementia, often quite dramatically, there’s helpful information about the unique symptoms — which include hallucinations, delusions, and sleep issues — along with links to virtual support groups.
Excerpts:
- Regardless of the initial symptom, over time all three presentations of LBD will develop very similar cognitive, physical, sleep and behavioral features.
- Some individuals will start out with a movement disorder leading to the diagnosis of Parkinson’s disease, and later develop dementia. This is diagnosed as Parkinson’s disease dementia.
- Another group of individuals will start out with a cognitive/memory disorder that may be mistaken for AD (Alzheimer’s disease), but over time, two or more distinctive features become apparent, leading to the diagnosis of ‘dementia with Lewy bodies.
- Lastly, a small group will first present with neuropsychiatric symptoms, which can include hallucinations, behavioral problems, and difficulty with complex mental activities, also leading to an initial diagnosis of DLB. (Source: 10 Things You Should Know about LBD)
Now you know why it’s so confusing!
Alzheimer’s disease (AD)
Personal observations: Thanks to enhanced public education and courageous people like the Reagans and the Shrivers who have shared their experiences, most people are familiar with Alzheimer’s disease. Even so, almost everyone I’ve interviewed has described a bewildering and protracted struggle to arrive at a diagnosis. Susan Disney Lord, daughter of Roy E. Disney, talked with me about her mother’s years-long battle with confusion and disorientation before the family understood what was happening. You can hear her account in the Podcast section of this website.
Maria Shriver is someone I deeply admire as a woman, mother, and journalist. She’s also a tireless advocate for people battling Alzheimer’s. Check out Maria’s website here.
From the textbooks: Alzheimer’s is a degenerative disease that destroys memory and other important mental functions. At first, someone with Alzheimer’s may notice mild confusion and difficulty remembering details. Eventually, people may even forget loved ones and undergo dramatic personality changes. (Source: Mayo Clinic)
- Hippocampus (memory center of the brain)
- Parietal lobes (processing sensory information, such as taste, temperature, and touch)
- Temporal lobes (understanding speech/language)
Learn about the Ten Early Signs and Symptoms of Alzheimer’s disease
Learn more about genetic factors, APOE, testing, epigenetics: Alzheimer’s Disease Genetic Fact Sheet (Source: National Institute on Aging at the National Institutes of Health)
More information and help:
While the Alzheimer’s Association has numerous local chapters under the national umbrella, the following cities have disassociated with the national organization to better control funds raised and programs implemented:
Frontotemporal dementia (FTD)
Personal observations: At the time my husband began showing symptoms, he was an accomplished physician. He began having trouble speaking, reading, writing, multi-tasking — doing his job as dean of a medical school. But most disturbing to me was the change in his behavior. Paranoia crept in. He began exhibiting anomalous behaviors: lying, spending money recklessly, endangering our family. I didn’t know who he was anymore. My constant requests for him to see a doctor were met with accusations: I was the problem. Not until his colleagues from Yale confronted him — and discussed with me — the dramatic cognitive changes they’d noticed, did we see a doctor. Even then, a definitive diagnosis was elusive because it was so easy for him to appear perfectly normal and cover for himself (others joined this effort, believing they were helping).
From the textbooks: As opposed to the previous diseases, this one is named for its location in the brain. FTD refers to several conditions resulting from the progressive degeneration of the temporal and frontal lobes of the brain. Because these areas play a significant role in decision-making, behavioral control, emotion, and language, any of these can be disabled over time. It can strike when patients are in their thirties, forties, or fifties, when people are at the peak of their careers and raising families, often leading others to believe they’re suffering from a mid-life crisis. People with FTD are often misdiagnosed with psychiatric problems such as depression, manic-depression, obsessive-compulsive disease, or schizophrenia, and occasionally vascular dementia, Parkinson’s disease, or Alzheimer’s. (Source: UCSF Memory & Aging Center)
The Memory and Aging Center at the University of California, San Francisco is a leader in many fields, but is known for its expertise in FTD.
Frontotemporal dementia is often misdiagnosed as a psychiatric problem or, less frequently, as Alzheimer’s disease. But frontotemporal dementia tends to occur at a younger age than does Alzheimer’s disease, sometimes between the ages of 40 and 45. (Source: Mayo Clinic)
The Association of Frontotemporal Dementias changed its name to The Association of Frontotemporal Degeneration. Sometimes the illness is called Frontotemporal Lobar Degeneration, and the series of disorders associated with deterioration of the frontal lobes (decision-making and insight) and the temporal lobes (speech center of the brain, especially on the left side) are often referred to as Frontotemporal Disorders. To add another layer, the disease used to be called Pick’s for the doctor who first identified Pick bodies in the brain. (Personal note: The name changing makes me crazy.)
Vascular dementia
Personal observations: When I first heard that someone I knew who had been struggling with cognitive decline was diagnosed with Alzheimer’s disease, I thought, that’s not right. I’d spent enough time with her to know that her memory problems weren’t significant enough, though other abilities had been compromised. She had difficulty tracking a conversation, and she’d offered/agreed to stop driving after a couple of fender benders.
I kept saying it wasn’t Alzheimer’s, but my personal experience told me it wasn’t Lewy body dementia or FTD either. Her relatives gave permission to share the brain scans with a different neurologist, who quickly identified vascular dementia.
Important point: Reading scans (MRI, CT) is a complex mix of science, art, experience, and diagnostic abilities. Just because it’s medicine doesn’t mean that all physicians possess the same skills. Make sure you have electronic copies of everything, and don’t hesitate to obtain a second or third opinion.
This person’s family hired a part-time caregiver to help with daily necessities. But I urged them to consider moving her out of the single-family home with a steep staircase before an accident occurred, and researched viable possibilities. Nothing changed. After a shopping excursion one evening, she fell backwards down the stairs and ended up in the hospital. It took a while for me to understand that people will make adjustments in their families at their own pace, and there’s nothing you can do to alter it. Much of the time, family members disagree on these matters. In fact, I’ve never heard about — or experienced — a loved one’s dementia without a huge dose of family conflict. Try not to take it personally.
Thanks to her remarkable and resilient friend, she was able to make the most of her few remaining years with excursions and road trips and lots of laughter.
From the textbooks: Vascular dementia refers to progressive loss of cognitive functions caused by vascular injury (i.e. small strokes) within the brain. Symptoms of vascular dementia may be difficult to distinguish from Alzheimer’s disease. Problems with organization, attention, slowed thinking, and problem solving are present, while memory loss is more prominent in Alzheimer’s.
Not everyone who has had a major stroke will develop vascular dementia, but the risk for dementia is significantly higher in someone who has had a stroke. (Source: National Institute on Aging at the National Institutes of Health)
Key parts of the brain involved:
Wherever the strokes occur. Vascular dementia is caused by conditions that damage the blood vessels in the brain, depriving the brain of oxygen. This oxygen shortage inhibits the brain’s ability to work as well as it should. For example, stroke blocks blood flow to the brain, decreasing oxygen. However, high blood pressure, high cholesterol, and smoking also increase the risk of vascular dementia, which can occur alone or with Alzheimer’s disease. (Source: National Heart, Lung, and Blood Institute at the National Institutes of Health
Other illnesses that can cause dementia:
Corticobasal Syndrome (CBS) or Corticobasal Degeneration (CBD)
Progressive Supranuclear Palsy
Chronic Traumatic Encephalopathy (CTE)
A more comprehensive list of neurodegenerative diseases and other disorders that can cause dementia: (Source: UCSF Memory and Aging Center)
- Alzheimer’s Disease
- Amyotrophic Lateral Sclerosis
- Chronic Traumatic Encephalopathy
- Corticobasal Syndrome
- Frontotemporal Dementia
- HIV-Related Cognitive Impairment
- Huntington’s Disease
- Lewy Body Dementias
- Mild Cognitive Impairment
- Parkinson’s Disease DementiPosterior Cortical Atrophy
- Primary Progressive Aphasia
What does early-onset dementia mean?
Early onset occurs when dementia symptoms start before age 65. Sometimes it’s referred to as young-onset dementia. Early stage is different. It refers to severity (meaning symptoms are still mild), as opposed to the age at onset.
Frontotemporal dementia (FTD) is notorious for striking people in their 30s, 40s, and 50s, devastating parents raising young children and managing the apex of their careers.
Background
The material in this section was derived from many months of qualitative research with children who were living with a parent’s dementia. Those interviews are documented by primary authors Tiffany Chow, M.D. and Katherine Nichols in “When Dementia is in the House: Needs Assessment Survey for Young Caregivers,” published in the Canadian Journal of Neurological Sciences. Based on the research, Tiffany and Katherine also created a website that was translated into three languages by collaborators who wanted to help disseminate this critical information.
Documentaries & Movies
My subjective opinions of movies (even remotely associated with dementia):
Glen Campbell: I’ll Be Me (Netflix)
Documentary: Legendary singer and guitarist Glen Campbell goes on tour after he’s diagnosed with Alzheimer’s disease.
You’ll love his family’s love and honesty, as well as the patience the audience shows him. But even as he deteriorates in daily life, the way he’s able to tap into long-term (and muscle) memories to perform onstage is breathtaking.
Alive Inside (iTunes)
Documentary: The enduring power of music as the brain fades.
An uplifting film that won the Audience Award at the 2014 Sundance Film Festival. If you’ve ever wondered how you can you connect with someone suffering from severe dementia, this movie suggests one of the simplest, cheapest, and most remarkable ways to reach people through music. Research behind the approach is compelling, but patients’ reactions will bring tears to your eyes.
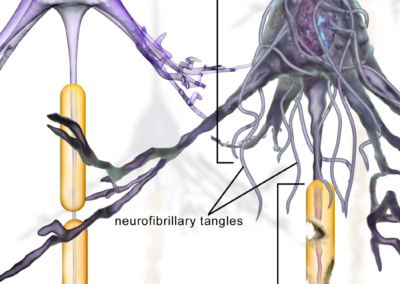
Can Alzheimer’s Be Stopped? (PBS on demand)
Documentary from Nova: Reporter Greg O’Brien reports on his own decline in an attempt to shatter stereotypes. It includes details about the latest research (plaques? tangles? genetic origins? environment?) and treatments, plus interviews with researchers from Genentech, as well as a physician who has treated families with early onset dementia, often beginning around age 45.
The Alzheimer’s Project (HBO)
An in-depth documentary series covering:
- The Memory Loss Tapes
- Momentum in Science
- Caregivers
- Grandpa, Do You Know Who I Am? — For kids
The science is heavy — the lineup includes leaders in these fields — and fascinating. But what really struck me (read: made me cry) were the interviews with the family members afflicted with the genetic mutation that guaranteed early onset Alzheimer’s. Their commitment to use their misfortune to help others is deeply moving.
Drama & Comedy
Still Alice (Netflix)
Drama: A Harvard professor battles early-onset dementia.
Actress Julianne Moore won an Oscar and a Golden Globe for her performance with an all-star cast that includes Alec Baldwin, Kristen Stewart, and Kate Bosworth. While the movie is good (how could it not be with these actors?), you may find it tilting toward the milder, prettier side of reality.
Away from Her (Hulu)
Drama: A man copes with his wife’s decline from Alzheimer’s disease.
A tender film about how cognitive decline ends a 40-year union. What’s not to love about Julie Christie’s performance? Here’s a comprehensive review from RogerEbert.com. Because he (or anyone working for him) does it better.
Know a movie or book you think should be included on the site? If so, please let me know the title and your opinion of its value.
Book Reviews
The objective is to honestly assess — not sell or slam — books on the market. The title will link to Amazon, because it’s easy for everyone, but feel free to support your local independent bookstore!
What if it’s Not Alzheimer’s? Edited by Lisa Radin and Gary Radin (2003/updated)
Revisions over the years (especially chapters on pharmaceutical therapies) sustain this book’s relevance as a guide to coping with any type of dementia. My first read, I’ll admit, frustrated me. But my husband had just been diagnosed with Frontotemporal dementia, and I felt like the victim of a hit-and-run, lying in the street mumbling what just happened? (or something less polite) after getting clipped by an 18-wheeler. Nothing gave me the information I wanted: How to help my husband get well. On some level, everything seemed too basic, confusing, irrelevant, or inadequate. But when I circled back, I wished I’d been able to absorb more content initially. Good stuff here.
What I like:
It begins with a concise overview of different types of dementia, The structure is clear (Part 1: Medical; Part 2: Managing Daily Care; Part 3: Caregiver Resources), each section has a distinct focus, and chapters are written by a cadre of notable scientists and physicians — all leaders in the field.
Excerpts:
…one of the most important differences between the frontotemporal dementia syndromes and Alzheimer’s disease is that the frontal dementias primarily affect behavior, often early and severely. It is this factor, perhaps more than any other, that makes caring for a frontal dementia sufferer so much more of a challenge.
* * *
Loss of self-awareness is one of the hallmarks of FTD…. In fact, when frontal dementia patients are asked to describe their current personality and behaviors, many will state that there is “nothing wrong with them” and will describe themselves as they once were, even misreporting factual information about themselves.
* * *
It is important to realize that this is not a case of psychological denial, as if the patient refuses to admit changes that could be perceived as shortcomings. This is, in fact, a brain-based disorder that prevents patients from accurately perceiving and interpreting new information about their behavior that would challenge their longstanding self-image.
A caregiver’s attempts to hold up a mirror to the patient will often result in escalating a fruitless power struggle.
* * *
This lack of insight actually presents much more of a burden for the caregiver than for the patient, who is oblivious to what would probably be devastating information about their progressive loss of abilities and the dramatic change from their previously held standards of behavior.
* * *
You are loving someone, living with someone, looking at someone who has become somebody else. This requires a tremendous supply of courage to keep going forward.
* * *
Instead of getting over it, which seems impossible because it is, those who are experiencing a great loss need to “get on with it.” This simply means getting on with life: as it is, each minute, each hour, each day.
* * *
Life is what you do with fifteen minutes.
Podcasts & Videos
The objective is to honestly assess — not sell or slam — books on the market. The title will link to Amazon, because it’s easy for everyone, but feel free to support your local independent bookstore!
Dementia in the House
Dementia in the House is a new podcast featuring brief (three to 15-minute) conversations with physicians, research scientists, family members, colleagues, attorneys, social workers, helpline coordinators, hospice nurses, end-of-life experts, patients, and anyone else who might have an interesting story, innovative solution, or fresh perspective.

Dementia in the House: Episode 1
Susan Disney Lord, granddaughter of Roy O. Disney (Walt’s brother), and daughter of Roy E. and Patricia Disney, shares details of her mother’s battle with Alzheimer’s disease, and her commitment to the board of Alzheimer’s Los Angeles (9:15):

Dementia in the House: Episode 2
Behavioral neurologist Tiffany Chow, M.D. explains the global clinical trials of USC’s Alzheimer’s Therapeutic Research Institute (3:53):

Dementia in the House: Episode 3
Nora Rahimian is the helpline coordinator at Alzheimer’s Los Angeles. Here’s how she responds to people calling for advice and compassion (6:00):

Dementia in the House: Episode 4
It’s easy to go along with a dementia patient’s alternative universe — until statements become allegations and ideas turn frightening and painful. On several occasions, my husband accused my son of stealing personal items. My father believed people were breaking into the house in the middle of night, and thought his wife was having an affair with one of his closest friends. What’s the most effective way to handle these situations? Behavioral neurologist Tiffany Chow offers suggestions that begin with doing whatever you can to help the patient feel safe, loved, happy, and healthy (please note: we’re not saying it’s easy!) 8:00:
Music
Making a Perfect Yesterday
Mahalo to ukulele virtuoso Jake Shimabakuro for granting permission to use his song “Making a Perfect Yesterday” for these podcasts and videos. Be sure to check out the entire album, entitled Dragon.
Videos
Scientists in Cars Talking About Brain Illness
…and maybe singing karaoke and getting coffee
“Scientists in Cars Talking about Brain Illness” is a video series inspired by Jerry Seinfeld’s Comedians in Cars Getting Coffee (Netflix) and James Corden’s “Carpool Karaoke” on the Late Late Show (CBS). You’re right: this won’t be as funny.
Episode 1: A wide-ranging conversation about dementia, Alzheimer’s disease, Lewy body dementia, Robin Williams, Parkinson’s disease and Parkinsonism (what’s the difference?), and Frontotemporal dementia with behavioral neurologist Tiffany Chow, M.D.
Please go easy on us. We’re doing the best we can without celebrities, a support crew, and stops for coffee in hip cafes!

Featuring Jake Shimabukuro’s “Making a Perfect Yesterday,” “Somewhere Over the Rainbow,” by Israel Kamakawiwo’ole, and Dr. Chow playing “Rainbow Connection” on her ukulele.
Rainbows and dementia. We’re determined to find hope and humor in it all.
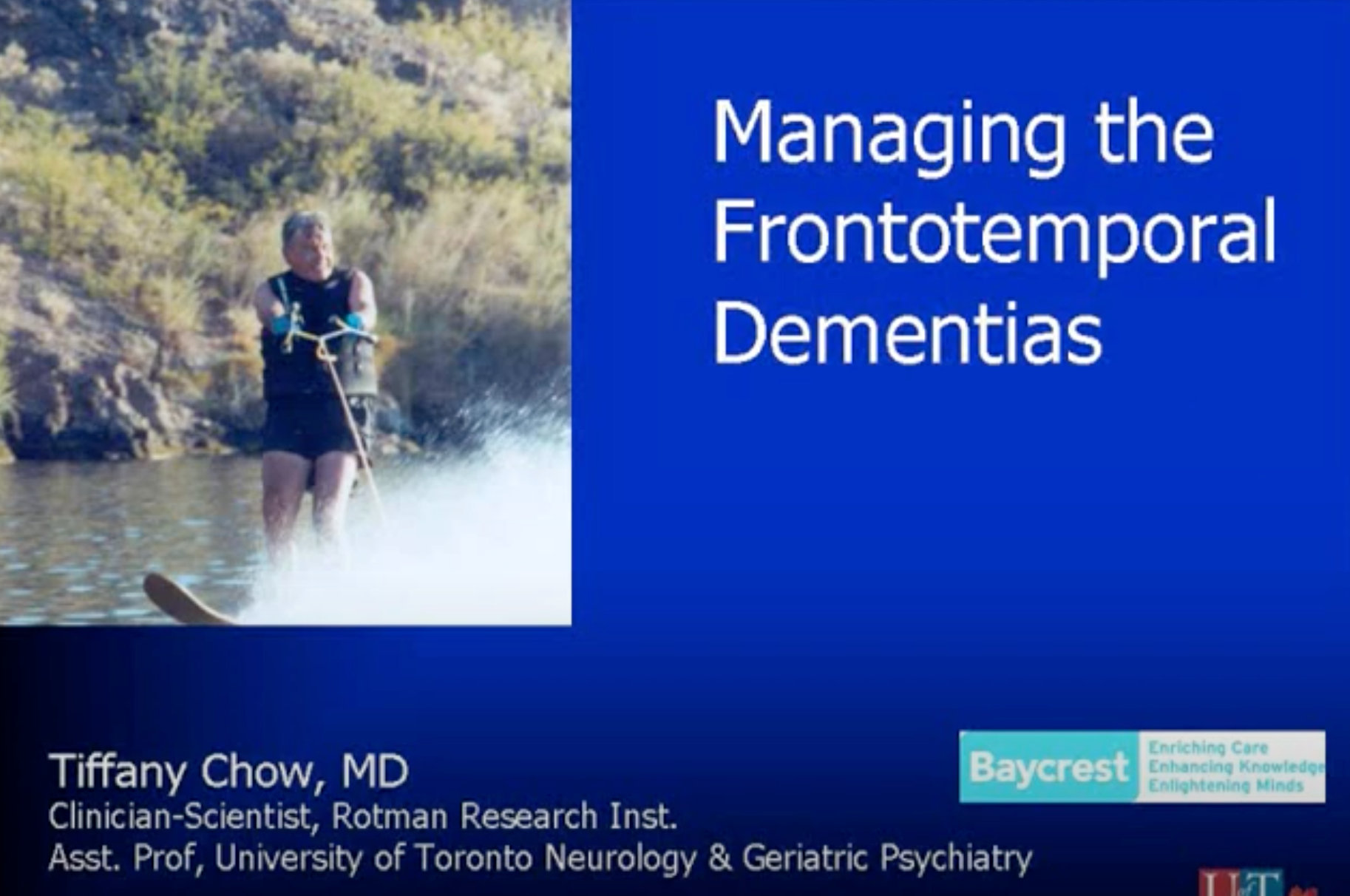
Managing Frontotemporal Dementia Through Caregiver Support
Tiffany Chow, M.D. gave this talk, which includes random clips of me, to a group of neurologists. One special note to physicians in this presentation: If we talk about our relationship with you, we don’t expect you to become a marriage counselor. We’re trying to illustrate how our loved one has changed, and why it affects every aspect of our lives. Yes, this was a response to personal experience in a doctor’s office.
Part 1:
Part 2: